
The novel coronavirus SARS-CoV-2, which causes the disease COVID-19. /NIAID-RML/AP
The novel coronavirus SARS-CoV-2, which causes the disease COVID-19. /NIAID-RML/AP
Yvon Chouinard is a fascinating man, an octogenarian billionaire environmentalist rock climber who gave the world one of its most famous inspirational quotes: "Fear of the unknown is the greatest fear of all." Chouinard's epigram graces a thousand inspirational posters but it has hard scientific implications: the more we know about a disease, the more we can combat or control it.
Coronaviruses get their name from the Latin corona – meaning crown, which they resemble under a microscope. The coronavirus family has seven strains known to infect humans. Four of them cause common colds; the other three lead to deadly infections including Middle East Respiratory Syndrome (MERS), Severe Acute Respiratory Syndrome (SARS) and COVID-19.
00:27
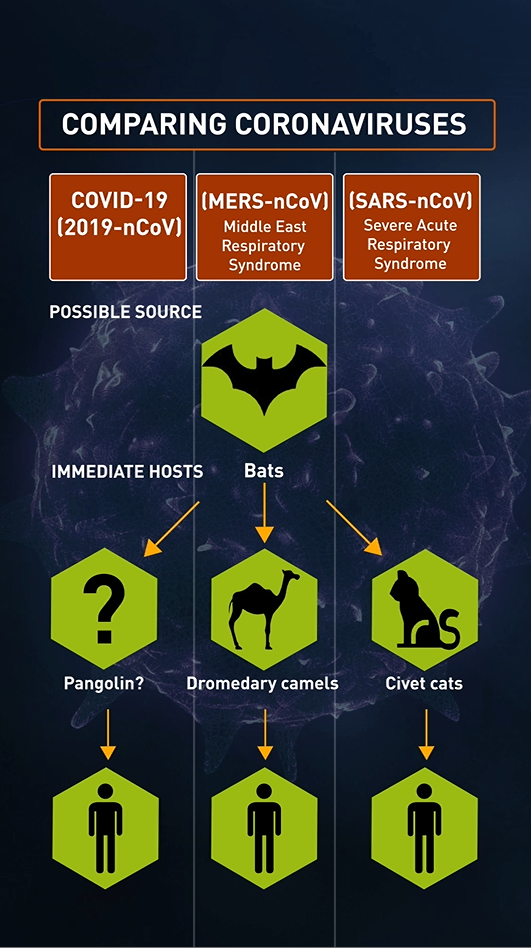
Coronaviruses are zoonotic, meaning they are transmitted from animals to humans. The SARS-CoV virus is believed to have been transmitted from civet cats to humans, while MERS-CoV probably traveled from dromedary camels to humans, but in both cases the original hosts seem to have been bats, which can often survive quite happily as the hosts for various viruses.
Many believe that SARS-CoV-2, the virus that leads to the disease now known as COVID-19, was also transmitted through another animal host. Science puts these viruses in the same category but where COVID-19 differs is that it spreads more quickly between humans – and has rapidly transferred itself across the world.
00:49

The enemy within
For most who contract COVID-19, the disease appears mild; counterintuitively, that's one of the things that makes it so deadly in the long run.
It takes about five days for the SARS-CoV-2 virus to establish itself in the human body, during which time a person will show no symptoms and may not even get sick for a surprisingly long time: the World Health Organization (WHO) has reported that the incubation period can last up to 14 days.
Living inside its unknowing hosts, this clever little ball of amino acids and proteins, which measures 80 billionths of a meter in diameter, can be transported around the world totally undetected.
About 80 percent of patients experience mild symptoms such as a fever or a persistent, initially dry, cough. Some report a sore throat, headache, tiredness and diarrhea, while there is some anecdotal evidence of a loss of smell and taste. This stage lasts about a week, after which most bodies' immune systems recover after rest and pain relief, such as paracetamol.

A medical staffer gives the thumb up sign to a patient in the ICU of the Bassini Hospital, near Milan, Italy. /Claudio Furlan/LaPresse/AP
A medical staffer gives the thumb up sign to a patient in the ICU of the Bassini Hospital, near Milan, Italy. /Claudio Furlan/LaPresse/AP
If these symptoms sound familiar, that's precisely the point. Coronavirus is very good at disguising itself as regular flu, ensuring maximum communicability by hiding in plain sight.
For more serious cases (about 14 percent), hospital treatment is required when a patient develops complications such as difficulty breathing because the virus primarily attacks the lungs. Checks will be carried out and oxygen may be given.
About six percent of coronavirus cases become critical, as the virus spirals out of control and causes pneumonia and multi-organ failure. This requires immediate intensive care. Patients will be put on ventilators, where oxygen is pushed into the lungs via a tube in the mouth, nose or through a small cut in the throat to keep the body alive.
Although figures change all the time, COVID-19 patients put on ventilators seem to have a 50 percent chance of survival: an NHS study in the UK reported a 66 percent death rate.
The majority of patients who die from the disease are described as having underlying health problems but this can include high blood pressure, obesity and diabetes – conditions that are common in many populations.

An electron microscope image of SARS-CoV-2, the coronavirus that causes COVID-19, shows the extruding peplomers, which resemble a crown. /NIAID-RML/AP
An electron microscope image of SARS-CoV-2, the coronavirus that causes COVID-19, shows the extruding peplomers, which resemble a crown. /NIAID-RML/AP
[The disease] can attack almost anything in the body with devastating consequences... its ferocity is breathtaking and humbling
- Harlan Krumholz, Yale University and Yale-New Haven Hospital
With the number of confirmed cases surging into the millions globally and deaths in the hundreds of thousands, clinicians and scientists are beginning to discover the extent of the damage wrought by COVID-19 as it engulfs the body. The media has concentrated on the more easily perceptible damage the diseased does to the lungs, as patients arrive at hospital gasping for air or lie helpless on ventilators. It is becoming apparent, however, that the virus has a deadly reach far beyond the lungs and that it can compromise many organs including the brain, gut, kidneys, blood vessels and heart.
It appears the body's response to the virus can injure many other organs. This means that damage to the population's health from COVID-19 could be worse than previously thought. In late March, JAMA Cardiology documented heart damage in nearly 20 percent of patients out of 416 hospitalized for COVID-19 in Wuhan, China. In another Wuhan study, 44 percent of 138 hospitalized patients had arrhythmias.
The scramble for ventilators by governments may soon be replaced by a scramble for dialysis machines as COVID-19 causes renal failure and kidney damage in a significant percentage of patients.
In the words of cardiologist Harlan Krumholz of Yale University and Yale-New Haven Hospital, who is gathering clinical data on COVID-19: "[The disease] can attack almost anything in the body with devastating consequences... its ferocity is breathtaking and humbling."
04:35

Comparing reproductive numbers
To understand any disease, it's vital to establish its reproductive number, or R-zero: how many new infections a single infectious individual will cause on average if left unchecked. The goal for any pandemic control is to reduce this to below one, ensuring the spread will slow until the disease dies out.
00:31
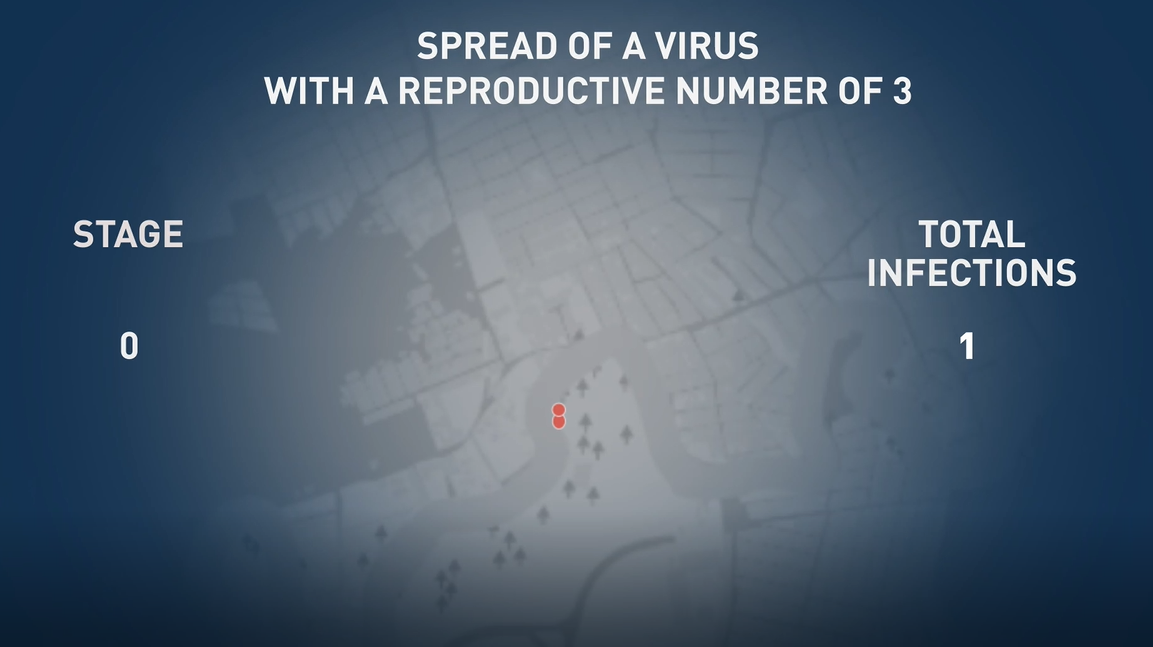
The WHO currently classifies COVID-19's R-zero as 2.5: so one person infects 2.5 people, each of whom in turn infects 2.5 people and so on. After 10 stages of transmission, this would result in more than 15,000 cases from the one original carrier.
The European Centre for Disease Control (ECDC), however, puts the R-zero at 3. Even such a small increase would result in almost 90,000 cases after 10 stages of transmission.
COVID-19 is very transmittable among humans. Swine flu was also highly transmittable, but the mortality rate was much less. That's why we have such severe measures coming into place
- Mike Tildesley, associate professor of infectious diseases at Warwick University
How it spreads
Like most cold and flu bugs, COVID-19 chiefly spreads via the average of 3,000 droplets dispersed when a person coughs or more than 10,000 from a sneeze. (To a greater or lesser extent, we also disperse droplets when we talk.)
These virus-laden droplets can be passed from person to person either by physical contact such as shaking hands; from contaminated hard surfaces, where the virus can survive for days; or by breathing in the droplets which hang in the air.
COVID-19 has been so successful because of its relatively high communicability. By the standards of lethal pandemics, its mortality rate – estimated by the WHO to be as low as 2 percent but recently pegged by Johns Hopkins University at 6.7 percent – isn't all that high. But that works in its favour: most of its carriers survive to spread the virus, especially during the disease's relatively lengthy asymptomatic incubation period.

A patient undergoes treatment in an intensive care unit (ICU) in Badalona, Spain /Felipe Dana/AP Photo
A patient undergoes treatment in an intensive care unit (ICU) in Badalona, Spain /Felipe Dana/AP Photo
By comparison, someone infected with SARS, which has a similar R-zero to COVID-19 but a higher mortality rate (estimated at 9.5 percent), was only contagious several days after symptoms appeared – making precautionary isolation far easier than with COVID-19.
The 2009 H1N1 pandemic, commonly known as swine flu, infected a huge number of people – some estimates go as high as 1.4 billion – but a very low 0.03 percent mortality rate. Meanwhile, although diseases like Ebola and MERS are more lethal, with mortality rates of 50 and 34.4 percent respectively, they were harder to contract and therefore easier to control.
"COVID-19 is very transmittable among humans," Mike Tildesley, associate professor of infectious diseases at Warwick University, told CGTN Europe. "Swine flu was also highly transmittable, but the mortality rate was much less. That's why we have such severe measures coming into place."
We may have several strains of this virus, some very aggressive, others much milder
- Kari Stefansson, CEO of Icelandic genetics company deCODE
Worryingly, COVID-19 has also found a way to mutate.
"The mutational pattern becomes specific for specific regions," Kari Stefansson, CEO of Icelandic genetics company deCODE told CGTN Europe. "One is relatively specific for Austria and another for Italy, a third for England and a fourth for the west coast of the United States."
Stefansson believes this could be why some patients experience just a mild cold, while others end up in hospital or dead.
"We may have several strains of this virus: some very aggressive, others much milder. Or it could be our genetic vulnerability: some of us are just born more resistant to this virus than others."
01:29

Super-spreading events
A reproductive number can only ever be an average. Due to conditions including population density, risk underestimation and the concentration of vulnerable people in one place – such as a care home for the elderly – some people will spread COVID-19 more than usual.
The term "super-spreaders" initially referred to people, but it has come to describe events which have caused a spike in a disease. According to the National Academy of Sciences and The London School of Hygiene & Tropical Medicine, three percent of cases of Ebola were responsible for 61 percent of infections.
In early- to mid-March, France held local elections, Milan fashion week took place in Italy's worst-affected Lombardy region and the UK's Cheltenham Festival attracted 250,000 racegoers, despite the increasing awareness of COVID-19. All these events have been held responsible for unnecessarily spreading the disease.

On 11 March, 3,000 Atletico Madrid fans traveled from the Spanish capital – where hundreds of cases had already been reported and schools were closed – to Liverpool for a Champions League match. Madrid's mayor later called it a 'mistake' to allow travel. /Jon Super/AP Photo
On 11 March, 3,000 Atletico Madrid fans traveled from the Spanish capital – where hundreds of cases had already been reported and schools were closed – to Liverpool for a Champions League match. Madrid's mayor later called it a 'mistake' to allow travel. /Jon Super/AP Photo
Super-spreading events have the largest influence on an outbreak's early trajectory
- Justin Lessler, Johns Hopkins Bloomberg School of Public Health
Yet a super-spreading event doesn't have to be a one-off occurrence. An average of 5.5 million people ride the New York City subway each day, the vast majority of them touching metal surfaces which we now know can harbour the disease for days. This and every other transit system worldwide may well be an example of an ongoing super-spreading event.
"Super-spreading events have the largest influence on an outbreak's trajectory early on. If there's only a few cases and one person then infects 10 others, it can make it start strong," said Justin Lessler, an associate professor of epidemiology at the Johns Hopkins Bloomberg School of Public Health.
Like every other virus, SARS-CoV-2 exists to replicate; like the most successful viruses, it finds ways to live in its hosts rather than kill them, otherwise it dies, too. MERS and Ebola were just too lethal.
This is where COVID-19's genius lies. Because it's not deadly enough to kill its hosts immediately, and it doesn't make its presence known until much later, people don't fear it in its early stages. Once you're scared, it may already be too late.
