
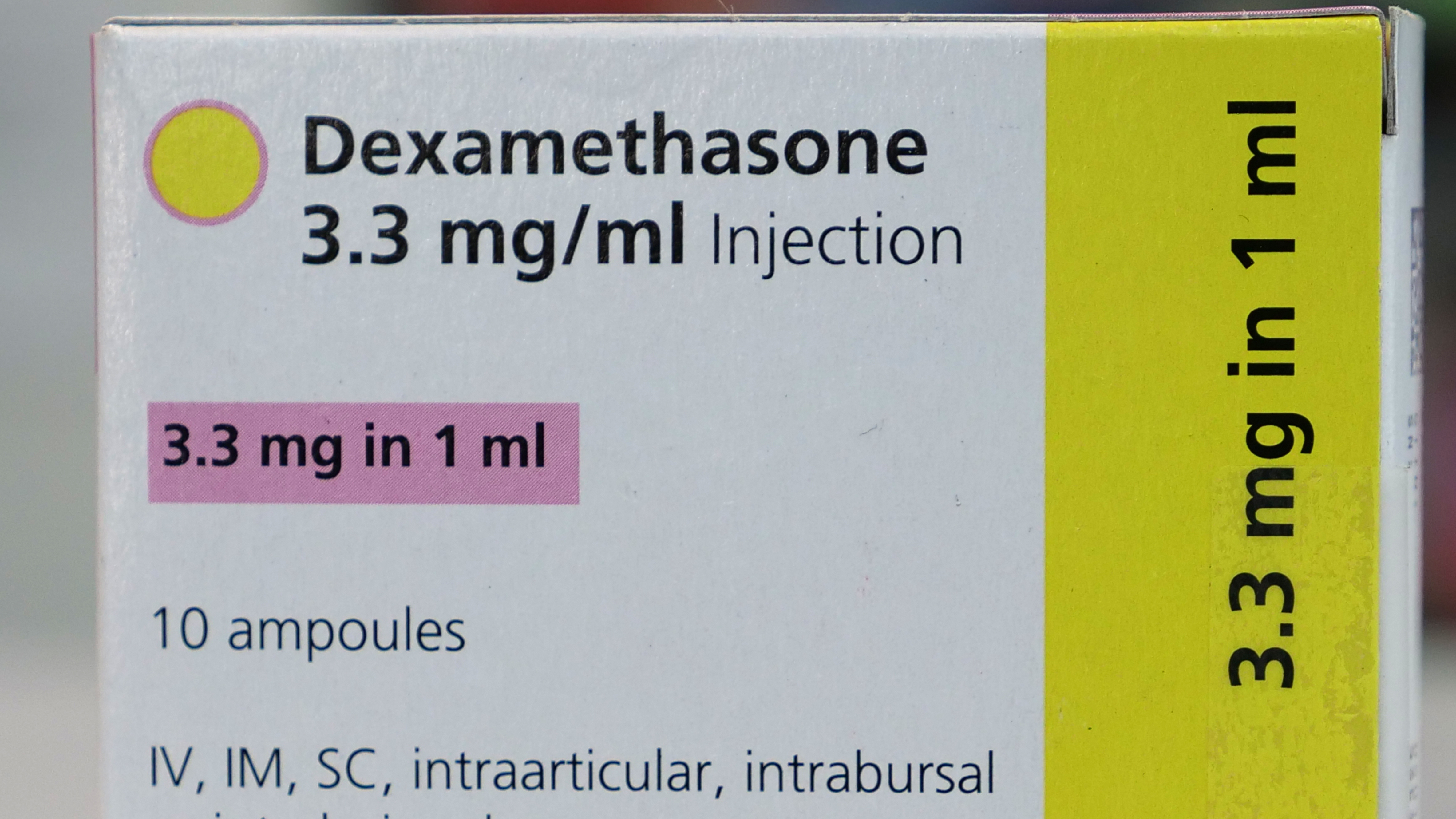
Dexamethasone is an easily available and relatively cheap drug. /Justin Tallis/AFP
Dexamethasone is an easily available and relatively cheap drug. /Justin Tallis/AFP
Dexamethasone is being championed as the first coronavirus drug that saves lives and while there is plenty of optimism, some scientists say further testing still needs to be done.
The steroid, which is used to reduce inflammation, has lowered the death rate of severely ill COVID-19 patients by a third in trial results announced on Tuesday.
The Oxford University RECOVERY trial compared outcomes of around 2,100 patients who were randomly assigned to get the steroid, with those of around 4,300 patients who did not get it.
While the breakthrough has been celebrated in the UK, in the U.S. and Russia it has been welcomed more skeptically.
What is dexamethasone?
Primarily a drug that is used to reduce inflammation, dexamethasone has been used in the treatment of conditions including allergies, asthma, eczema and arthritis. It is also administered in end-of-life care and is effective in preventing the immune system from destroying blood platelets in people with blood disorders. It can reduce the swelling for people suffering from brain tumors.
When was it created?
It was developed in 1957 and was first approved for medical use in the U.S. a year later. During the 1960s it began to be widely used.
Who conducted the COVID-19 trial using dexamethasone?
The Oxford University RECOVERY trial was launched in April as a randomized clinical trial to test a range of potential treatments for COVID-19, including low-dose dexamethasone and the malaria drug hydroxychloroquine.
The hydroxychloroquine arm was halted earlier this month after it was found to be ineffective in the treatment of the coronavirus. The trial compared outcomes of around 2,100 patients who were randomly assigned the steroid with those of around 4,300 who didn't get it.
Scientists say the drug can reduce by a third the deaths of critically ill patients. /Arman Soldin/AFP
Scientists say the drug can reduce by a third the deaths of critically ill patients. /Arman Soldin/AFP
How big a breakthrough is this?
The trial has found that the drug reduces the mortality rate by around a third for patients who are critically ill with COVID-19.
It means that for those put on ventilators, one death would be prevented in eight, while one in 25 for people who require oxygen alone.
A big bonus of the drug is that it is available and relatively cheap as the treatment for each patient would be likely to cost less than $50. While it is on the U.S. Food and Drug Administration's list of drugs in shortage, suppliers including Germany's Fresenius say they have the drug readily available.
What do fellow scientists say?
There has been plenty of positivity about the use of the drug but also caution.
"We have been burned before, not just during the coronavirus pandemic but even pre-COVID-19, with exciting results that when we have access to the data are not as convincing," said Kathryn Hibbert, director of the medical intensive care unit at Harvard's Massachusetts General Hospital.
Hibbert said published data would help her evaluate the findings and see which patients benefited the most and at what dose.
"I am very hopeful this is true because it would be a huge step forward in being able to help our patients," she said, but added she would not change practice at this point.
Her view was echoed by Mark Wurfel, professor of medicine at the University of Washington, who added: "This magnitude of improvement in mortality for a critically ill population is about the largest effect size that we've ever seen."
Other scientists also wanted to see the published data.
"We hope the data on which these results are based will be published as soon as possible so that doctors can confidently put the treatment into practice," said Robin Ferner, honorary professor of clinical pharmacology at the University of Birmingham.
Thomas McGinn, deputy physician-in-chief at Northwell Health, New York's largest healthcare system, told Reuters that physicians at Northwell hospitals have been using steroids on a case-by-case basis because they can suppress patients' immune systems and possibly make them susceptible to other infections.
He said that if the data are peer-reviewed and legitimized, it could spread the use of steroids in the sickest COVID-19 patients.
"Across the country now, intensivists have been using it based on their judgment calls. If this is legitimate, you may find ... instead of say five out of 10 intensive-care COVID patients getting it, maybe everybody would get it," McGinn said.
Meanwhile, Russian health ministry official Sergei Avdeev has told RIA news agency that the country already uses dexamethasone to treat patients but disagrees it is a panacea.